WOMEN VETERANS HEALTH IN 2026: THE BREAKTHROUGHS, BARRIERS, AND POLICY SHIFTS YOU NEED TO KNOW
COMMENT
SHARE

Every woman Veteran has a story, many of which involve challenges with the VA system. Sarah, a decorated Air Force pilot, struggled to find healthcare that met her unique needs. She often faced dismissals and lacked resources for her post-service health issues.
Now, in 2026, this narrative is shifting. Ask any woman Veteran what she wishes the VA better understood, and you'll hear striking consistency. The health burdens women carry from service are heavier, more layered, and often misunderstood in a system built decades ago. But in 2026, women Veterans are no longer at the margins of VA care; they’re shaping it.
This year stands out for expanded services and the alignment of advocacy, data, and policy. For years, women Veterans voiced their needs. Now, the VA is visibly responding. Yet, progress highlights persistent gaps. Next, we'll examine how the system adapts to evolving needs.
A System Catching Up to the Fastest-Growing Veteran Population
Women Veterans, now over two million nationwide, are the fastest-growing Veteran group. This growth compels the VA to adapt primary care, specialty services, and mental health to meet changing needs.
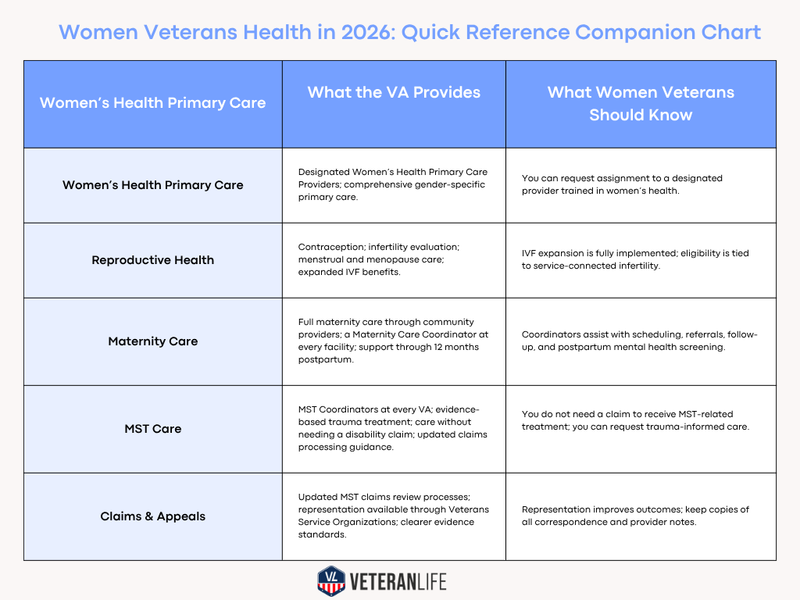
The VA’s model now ensures every enrolled woman Veteran can access a designated women’s health primary care provider. These clinicians deliver gender-specific care, including contraception, menopause management, cervical cancer screening, breast health, chronic disease management, and mental health integration.
Women’s health hubs continue expanding across the country, with more VA medical centers upgrading mammography equipment, strengthening coordination between primary and specialty care, and building teams trained in women’s health. Same-day mental health access has become standard at many facilities, offering quicker entry points during urgent situations.
Still, access is uneven. Staffing shortages, little OB-GYN availability, and rural gaps make wait times and travel unpredictable. Across the nation, median wait times can vary significantly, with some women Veterans waiting up to three times longer than those in urban areas, underscoring regional disparities. For women Veterans, care quality often depends on their ZIP code.
“Women Veterans are the fastest-growing population in the VA, and their care has to grow with them.”
Reproductive Health Access: What 2026 Brings Into Focus
Reproductive health is one of the most rapidly evolving areas in female Veterans’ care. The VA already offers contraception, infertility evaluation and management, menstrual and menopause care, and preconception counseling. But the most significant shift came with the 2024 expansion of in vitro fertilization for eligible veterans with service-connected infertility.
Under this expansion, eligible Veterans can receive IVF regardless of marital status, and for the first time, donor eggs, sperm, or embryos can be used when medically necessary due to service-connected conditions.
This policy will be fully implemented in 2026.
Alongside fertility care, the VA’s Maternity Care Coordination Program is crucial. Every pregnant Veteran is assigned a coordinator to guide care, support scheduling, and provide follow-up through 12 months postpartum. This extended window is vital as postpartum depression and anxiety rates remain high nationwide.
Access remains hard. Maria, a Veteran in rural Montana, drives over three hours for standard appointments, highlighting the distance to community care. Inconsistent appointments drain time and resources. Reproductive health expanded, but accessing it still requires navigation skills many Veterans lack.
MST Care and Claims: How the System Is Changing and Where It Still Falls Short
Military sexual trauma is one of the most urgent health concerns affecting women Veterans. The VA defines MST as sexual assault or repeated, threatening sexual harassment experienced during service. Veterans can receive MST-related treatment without needing to file or be granted a VA disability claim, and this remains one of the most important protections available.
A decade of VA Inspector General reports revealed widespread inconsistencies in MST-related claims processing, from missing evidence requests to premature denials. In response, the VA centralized key parts of MST claim review, standardized training, and improved oversight. Grant rates for MST-related conditions have increased compared with earlier years, reflecting more accurate evaluations and stronger reviewer guidance.
Clinically, the VA provides evidence-based treatments for PTSD and trauma-related conditions, and MST Coordinators are present at every VA facility. Trauma-informed care initiatives have also grown, addressing privacy, environment, and clinical sensitivity.
But gaps remain. Claims vary in quality, appeals retraumatize survivors, and not all facilities have robust trauma-informed care. Women Veterans still seek consistency in paperwork and care.
“No survivor should have to navigate the system alone. MST care has to be consistent, trauma-informed, and timely.”
Mental Health, Chronic Conditions, and the Weight Women Veterans Carry
Women Veterans experience higher rates of depression, anxiety, PTSD, and chronic pain than non-veteran women. VA suicide prevention data shows that suicide among women Veterans decreased by approximately 17% between 2021 and 2022, an encouraging trend attributed to expanded crisis support, improved screening, and broader mental health access. But risk remains disproportionately high, and vigilance is essential.
Chronic conditions pose concern. VA research reveals higher rates of heart disease, chronic pain, autoimmune disorders, and injuries among women Veterans. Many also juggle caregiving, finances, and ongoing medical needs.
Chronic pain care is still among the least tailored. Earlier research focused on men, leaving service-related pain gaps for women. Many women Veterans feel unheard or undertreated.
Where Progress Stalls, and Why It Matters More Than Ever
Despite progress, access remains unequal. Specialty care, trauma-informed practices, and mental health vary by region. Rural women face long travels, limited options, and inconsistent VA coordination.
Transitioning from the Department of Defense (DoD) to the Department of Veterans Affairs (VA) within the first 90 days is often a critical challenge for newly separated women Veterans. The initial period is marked by inconsistencies in records transfer and gaps between TRICARE and VA care. During this time, many women Veterans must manage complex needs with limited support.
To address these challenges, here is a quick checklist to help navigate the DoD-to-VA handoff in those crucial early days:
- Ensure you have all necessary documents from your DoD service.
- Confirm transfer of medical records.
- Establish contact with a designated Women’s Health Primary Care Provider.
- Immediately connect with a VA representative for assistance with any access issues or questions.
This structured approach can ease the transition and promote smoother integration into the VA system.
These barriers impact real outcomes, delaying diagnoses and worsening chronic conditions.
“Progress is real, but parity is not here yet.”
What Women Veterans Can Do in 2026 to Advocate for Their Own Care
Now is the time for women Veterans to act. These strategies, rooted in current VA policy, empower you to take control of your healthcare journey and demand the level of care you deserve.
- Ask to be assigned to a designated Women’s Health Primary Care Provider. These providers receive specialized training in women’s health and can coordinate comprehensive care.
- Use the Women Veterans Program Manager for help with access issues, referrals, or concerns about services. Every VA medical center must have one.
- Use your Maternity Care Coordinator if you are pregnant or planning a pregnancy. They manage referrals, follow-up, and postpartum support through 12 months.
- Ask for printed or digital copies of imaging, lab results, and visit summaries. Keeping your own records helps with referrals, second opinions, and moving between systems.
- Request clarification on community care eligibility. Wait-time and drive-time standards determine whether you can receive non-VA care.
- Connect with a Veterans Service Organization to assist with MST claims or appeals. Representation can reduce administrative errors and improve outcomes.
- If you feel unsafe or overwhelmed, contact the Veterans Crisis Line. Early intervention leads to stronger follow-up support.
These steps don't excuse system flaws, but you can help make care more coordinated, safer, and more consistent now by putting them into action.
A Toolkit for Women Veterans Navigating VA Health Care in 2026
What to bring to every appointment:
- A current medication list
- Your latest imaging and lab results
- Questions about contraception, menopause, pain management, or fertility
- Any mental health concerns you want addressed
- Notes about symptoms, triggers, or care gaps you want resolved
Questions to ask your provider:
- Am I assigned to a Women’s Health Primary Care Provider?
- How do I access community care if needed?
- Who is my point of contact for test results or referrals?
- Do you offer trauma-informed care? What does that look like here?
- Can I receive a printed copy of today’s plan before leaving?
Who to contact for specific support:
- Women Veterans Program Manager
- MST Coordinator
- Maternity Care Coordinator
- Patient Advocate
- Community Care Office
This is navigation power, rooted in policy, resources, and authority.
The Pivot Point Still Needs Pressure
Women Veterans have waited decades to be seen, heard, and treated as central to the Veteran community. The momentum of 2026 is real. Expanded reproductive services, better mental health access, stronger MST reform, and dedicated women’s health teams reflect genuine progress.
But progress is not parity. And parity will not arrive without persistence.
Women Veterans carry the weight of service and the weight of a system still learning to serve them back. Their advocacy, individual and collective, is the force reshaping the VA. And in 2026, that momentum will finally start to match the magnitude of what women Veterans have carried all along.
Women Veterans Health in 2026: Quick Reference Companion Chart
Women Veterans Health in 2026: What to Do Today
- If you want better care, immediately: Ask to be assigned to a Women’s Health Primary Care Provider.
- If you’re pregnant or planning a pregnancy: Contact your Maternity Care Coordinator for scheduling, referrals, and postpartum support through 12 months.
- If you experienced MST: Request an MST Coordinator and trauma-informed care. You do not need a disability claim to receive treatment.
- If you’re struggling with mental health: Use same-day access options and ask your provider about evidence-based therapies for PTSD, depression, or anxiety.
- If you’re dealing with chronic pain: Request evaluation for chronic pain management and ask whether community care is available based on wait-time or drive-time standards.
- If you think you qualify for fertility support: Ask about eligibility for the expanded IVF program for service-connected infertility, including donor options.
- If you need care sooner: Ask if you meet the eligibility requirements for Community Care. Wait-time and travel-time standards determine access.
- If something goes wrong with your appointment or referral: Contact your Women Veterans Program Manager or Patient Advocate.
- If you’re filing or appealing a claim: Get representation from a Veterans Service Organization. It reduces errors and improves claim outcomes.
- If you want your care to follow you: Request printed or digital copies of your labs, imaging, referrals, and visit notes.
Suggested reads:
Join the Conversation
BY NATALIE OLIVERIO
Veteran & Senior Contributor, Military News at VeteranLife
Navy Veteran
Natalie Oliverio is a Navy Veteran, journalist, and entrepreneur whose reporting brings clarity, compassion, and credibility to stories that matter most to military families. With more than 100 published articles, she has become a trusted voice on defense policy, family life, and issues shaping the...
Credentials
Expertise
Natalie Oliverio is a Navy Veteran, journalist, and entrepreneur whose reporting brings clarity, compassion, and credibility to stories that matter most to military families. With more than 100 published articles, she has become a trusted voice on defense policy, family life, and issues shaping the...